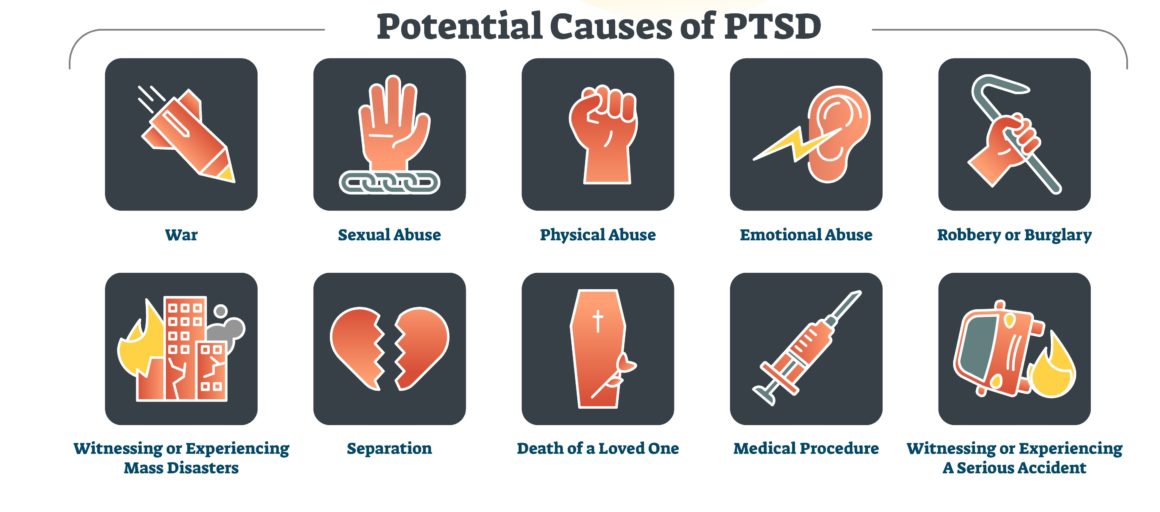
Whether it’s a bad accident, a history of military service or a traumatic personal experience such as assault or even a psychological breakdown, post traumatic stress disorder (PTSD) can quickly become a part of an average person’s life. The ongoing effects of PTSD can have significant cognitive consequences.
PTSD is defined in the Diagnostic and Statistical Manual as trauma caused by exposure to an event involving “actual or threatened death, serious injury, or threat to one’s physical integrity.” It’s estimated that one-in-eleven American adults experience PTSD in their lifetime, a fact that has significant implications for cognitive health.
Commonly recognized symptoms of PTSD include changes in cognitive processes such as memory, attention, planning, and problem solving. These factors can drive changes that impact negative emotionality, having a further effect on cognitive functioning.
The problem is common in populations you might suspect, such as veterans and medical personnel, but the reasons that cognitive impairment occurs is not clear. According to the U.S. Department of Veteran’s Affairs, there is not sufficient longitudinal evidence to determine the pathways through which PTSD impacts the development of neuro-cognitive function and risk for dementia.

What Research Exists?
An analysis published in The Journal of Neuropsychiatry and Clinical Neurosciences looked at 21 studies conducted between the years of 1968 and 2009. The conclusion was that “individuals with PTSD, particularly veterans, show signs of cognitive impairment when tested, more so than individuals exposed to trauma but who did not develop PTSD from it.”
Another study published in the journal Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring examined the effects of PTSD in 9/11 first responders. Researchers examined more than 800 first responders between January 2014 and April 2015 looking for signs of PTSD and depression, while also looking at medical data dating back to 2002. First responders were also screened for current symptoms of cognitive impairment.
Those who were present at the World Trade Center showed higher rates of PTSD, with 12.8% experiencing symptoms of cognitive impairment. Just over 1% of the participants showed signs of possible dementia. Both depression and PTSD were associated with symptoms of cognitive impairment, even after considering other physical and mental health factors that could contribute to it.
Those who suffered from recurring episodes such as flashbacks were more likely to suffer from cognitive impairment. Researchers concluded that about 20% of all 9/11 first responders eventually developed PTSD.
Increased Risk for Women
PTSD is twice as common in women as it is men. There is a number of reasons for this, from women making up the majority of the nursing workforce and therefore being exposed to trauma repeatedly, or the fact that women are more often the victims of sexual assault and abuse.

Research presented at the Anxiety and Depression Association of America (ADAA) conference in 2017 revealed that scientists had been examining nurses from the Nurses’ Health Study II, originally recruited in 1989. At the time of review in 2014, participants were between the ages of 49 and 69. What researchers concluded was that those with the most severe symptoms of PTSD had gone through the cognitive equivalent of four years of aging when compared to women who had experienced no trauma.
As you might expect, the older their age of the subject, the more the nurses cognitive performance had declined. The research was notable, however, in that it proved there is nothing unique about PTSD from combat, as the nurses showed very similar effects of PTSD found in male counterparts who suffered PTSD from military service. It also showed that the link between cognitive decline and PTSD was as true for the general population as it was for combat veterans.