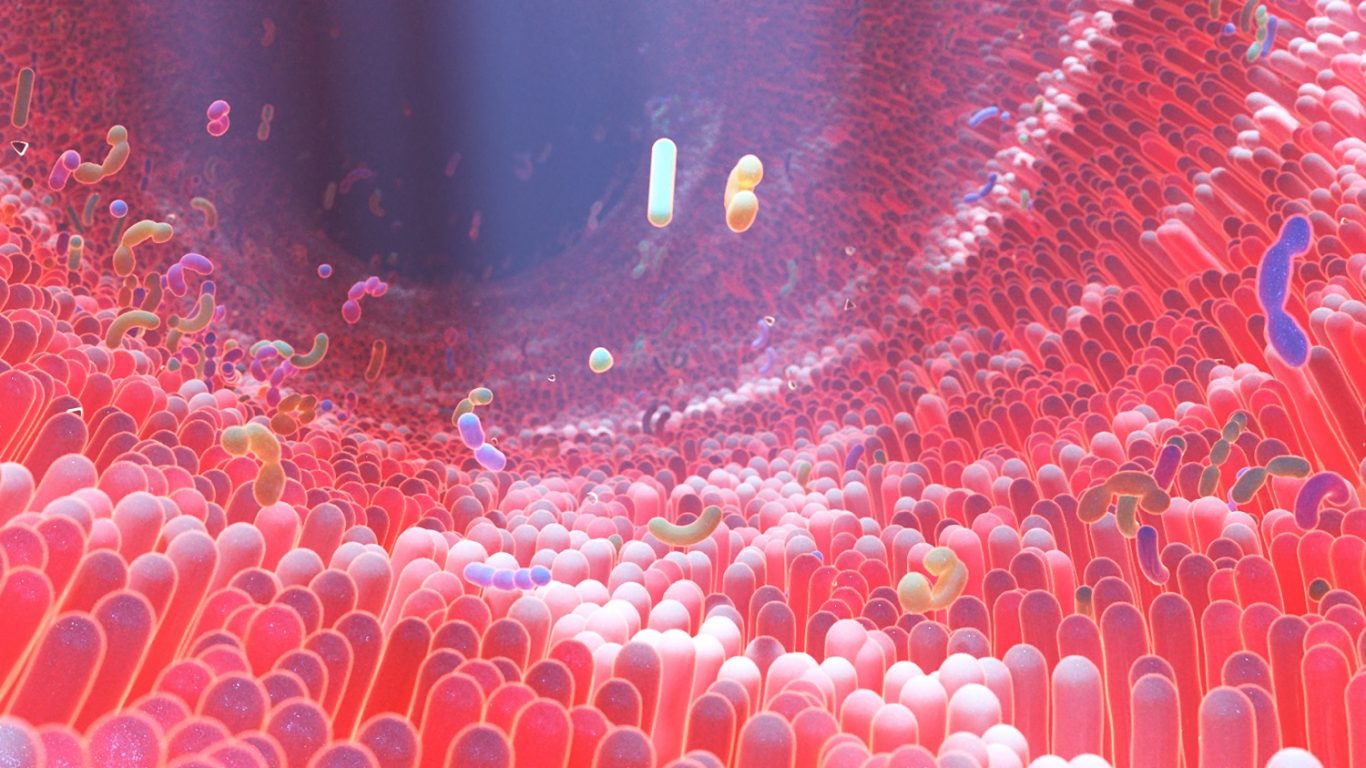
A new study has identified harmful bacteria in the gut that researchers believe plays a significant role in the development of Alzheimer’s, Parkinson’s, and other neurodegenerative diseases. They’ve also identified another type of bacteria that may help counteract this effect.
The new findings expand on previous research that has found an association between our mental health, cognitive function and changes in the gut microbiome. It also provides another reason for people to pay attention to the connection between their brain and gut – it can impact everything from mental health and neurodegenerative disease to anxiety and digestion issues.
“Looking at the microbiome is a relatively new approach to investigating what causes neurodegenerative diseases,” said Dr. Daniel Czyz, a University of Florida assistant professor and lead author on the study. “In this study, we were able to show that specific species of bacteria play a role in the development of these conditions.”
The Gut Bacteria Associated With Alzheimer’s and Parkinson’s
The researchers tested their theory using worms known as C. elegans. After infecting the worms with bacteria, proteins associated with diseases that impact cognition began to build up in their bodies. The C elegans also lost a great deal of mobility.
The bacteria that disrupted proteostasis, the process that regulates protein protection, is a pathogenic gram-negative bacterium. This “bad bacteria” is associated with the formation of protein tangles that researchers believe is a cause of Alzheimer’s disease and Parkinson’s disease.
But the researchers also found that another bacterium – butyrogenic bacteria – inhibited the aggregation of protein. Czyz said that recent studies have shown “patients with Parkinson’s and Alzheimer’s disease are deficient in these ‘good’ bacteria, so our findings may help explain that connection and open up an area of future study.”
That future study will likely include research into what forms these different types of bacteria and how dietary change and drug treatments can encourage the creation of more good bacteria.
The Strong Brain-Gut Connection
While the new research shines a light on the specific bacteria involved in the brain-gut connection, that connection has always been apparent. People know it’s there from the first day they think discover that just thinking about food can make their stomach rumble. The connection flows the other way, too.
As explained by Harvard Health: “A person’s stomach or intestinal distress can be the cause or the product of anxiety, stress, or depression. That’s because the brain and the gastrointestinal system are intimately connected.”
What causes changes in the gut microbiome is not always clear. Stress and anxiety can trigger issues in the gut, as can external factors such as air pollution, the quality of water we drink and drug and supplement use.
University of Florida research from 2020 also found that certain gut bacteria are present in people with depression, potentially opening up the possibility of using genetic profiling of gut bacteria to diagnose and treat depression. For example, some bacteria are responsive to antibiotics, which raises the possibility that antibiotics could be developed to target specific types of bacteria living in the gut microbiome of those with depression.
