Hyperbaric oxygen therapy (HBOT) sounds high tech, but in reality, it’s a treatment that has been the subject of research for decades. It can be used for a wide variety of medical conditions, ranging from diabetes to skin wounds and post radiation injuries suffered by cancer patients. Recently new potential has been found around treating brain injury and cognitive decline.
Also known as HBOT, hyperbaric oxygen therapy involves exposing the patient to a high-pressure environment containing oxygen levels of 100%. To give you an idea of how high that is, in the average room the blood oxygenation is around 100 mmHg, while the hyperbaric chamber both pressure and oxygen concentration are elevated so blood oxygenation can be increased to ≈ 1,500 mmHg (≈15 fold higher).

How does HBOT work?
Most of the healing processes depend on energy/oxygen- and therefore tissue hypoxia (oxygen deficiency) is the main reason for non-healing wounds. By raising the level of free oxygen in the blood, hyperbaric oxygen treatment induces angiogenesis (the creation of new blood vessels), enhances the proliferation of the cells that reconstruct the tissue (fibroblasts), increases generation of bones, and increases both the proliferation and release of stem cells to the circulation and the injured tissues. In addition, hyperbaric oxygen improves the anti-bacterial activity, both directly and indirectly.
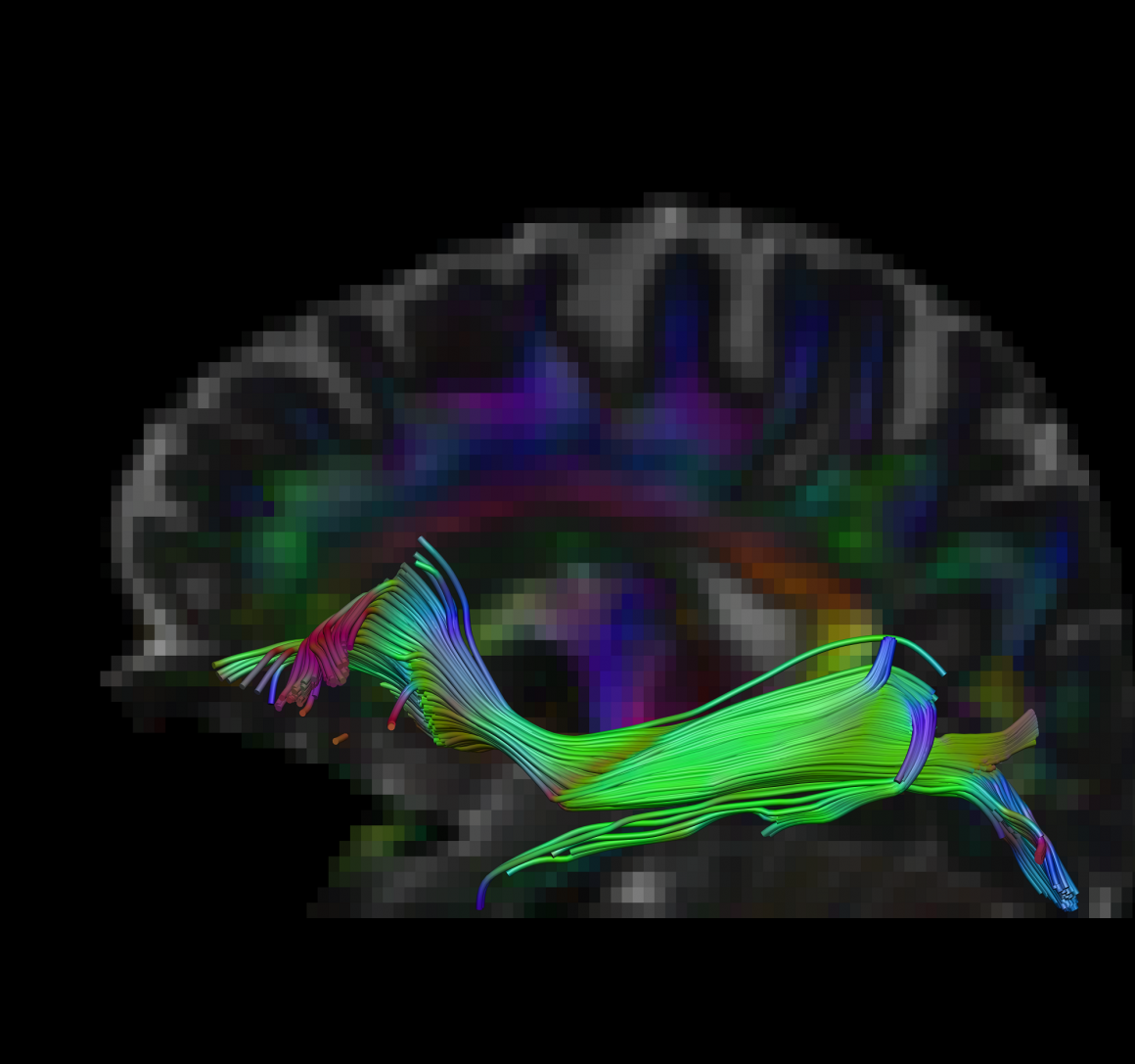
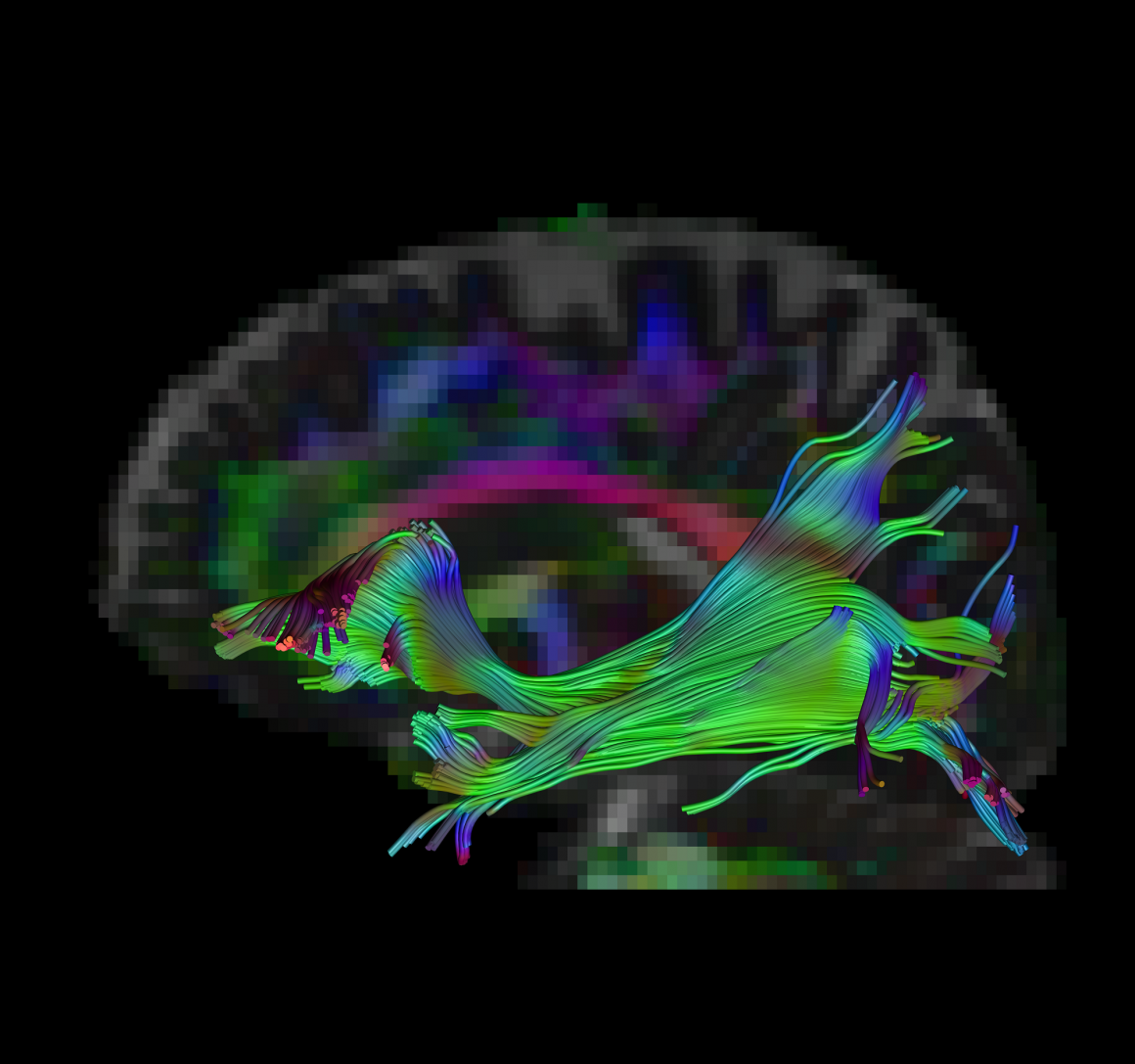
Brain Fibers – Pre HBOT Brain Fibers – Post HBOT
Even though many of the beneficial effects of HBOT can be explained by improvement of tissue oxygenation, it is now realized that intermittent increase of oxygen concentration can induce many of the mechanisms that are usually induced during hypoxia (lack of oxygen) but without the hazardous related hypoxia.
HBOT sessions
HBOT is a non-invasive treatment and is typically administered in an outpatient setting. Those who have been prescribed HBOT will need more than one session to enable an appropriate regeneration and recovery of the injured tissue with significant benefits. For example, according to the Mayo Clinic, those with nonhealing peripheral wounds may require as many as 20-40 visits, while those undergoing HBOT to induce neuroplasticity (neurons regeneration), recovery of an injured brain tissue, will required at least 40-60 sessions.

HBOT indications and future
The FDA has approved a number of uses for HBOT such as treating cases of decompression sickness, carbon monoxide poisoning and slow healing wounds or other skin conditions. Insurance companies will typically help with the cost of HBOT for the FDA approved indications.
Clinical studies published in recent years present convincing evidence that HBOT can be the coveted neurotherapeutic method for brain repair of neurological incidents like traumatic brain injury, stroke, anoxic brain damage and age-related cognitive decline. This new understanding leads to a paradigm shift in the way we refer to chronic brain injuries; these should be basically considered and treated like other non-healing wounds in other parts of the body.
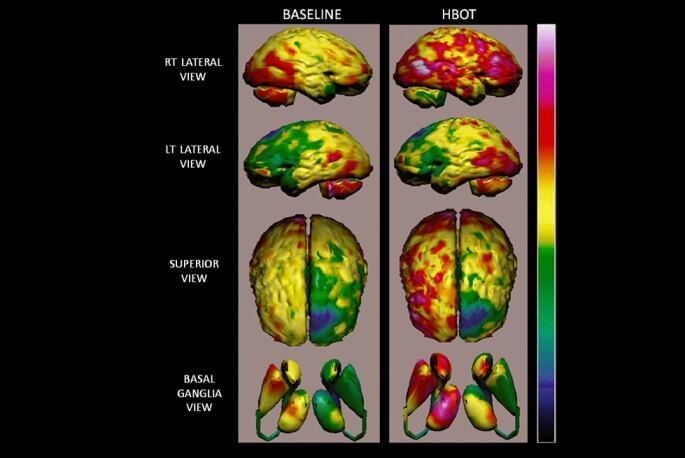
Current research suggests that HBOT can help to heal brain injury by restoring non-functioning neurons activity (neurogenesis) and connections side by side with the creation of new blood vessels. These studies show that HBOT can induce neuroplasticity (neurons regeneration) which leads to improved cognitive function of patients with malfunctioning brain regions.
Recent study, done on animal model of Alzheimer disease, demonstrated the beneficial effect of HBOT in reversing the pathogenesis leading to the disease. Interest in HBOT around the U.S. is growing thanks to its ability to address an array of age-related neurodegenerative conditions, such as cognitive decline.
As a result of all these potential benefits, there is also great interest in HBOT as a treatment in brain rehabilitation following head injuries, strokes and age-related cognitive decline.